The Idea of Checkpoint Blockade and the Cancer Immunotherapy Revolution
The immune system is a powerful network of cells in the human body that is essential for elimination of foreign invaders, such as bacteria and viruses. It has long been a dream of immunologists to harness the power of the immune system to attack tumors as well. Although this idea, called “cancer immunotherapy”, is very appealing, and has previously been shown to work in several mouse models of cancer, it has in general been very difficult to translate cancer immunotherapy approaches to humans. Because of this frustration, by the 1990s, many scientists and biotechnology companies had given up on the idea of cancer immunotherapy.
 Prof. James (“Jim”) P. Allison was not one of those that had lost hope. In the late 1990s, while serving as the Director of the UC Berkeley Cancer Research Laboratory, Jim became intrigued by a special biological molecule called CTLA-4. This molecule was displayed on the surface of particular cells in the immune system called T cells. Jim and his colleagues — most notably, graduate student Max Krummel, and postdoctoral fellow Cynthia Chambers — were able to provide evidence that CTLA-4 actually served to inhibit the activity of T cells. Since T cells were known to be critical for orchestrating immune attack, Jim and his colleagues hypothesized that perhaps one reason why T cells are not able to attack tumors is because they are being inhibited by CTLA-4. In a landmark Science paper published in 1996, Jim Allison, Max Krummel, and another postdoctoral fellow in the lab Dana Leach, showed that injection of mice with an antibody that blocks CTLA-4 could actually inhibit or eliminate tumor growth in the mice.
Prof. James (“Jim”) P. Allison was not one of those that had lost hope. In the late 1990s, while serving as the Director of the UC Berkeley Cancer Research Laboratory, Jim became intrigued by a special biological molecule called CTLA-4. This molecule was displayed on the surface of particular cells in the immune system called T cells. Jim and his colleagues — most notably, graduate student Max Krummel, and postdoctoral fellow Cynthia Chambers — were able to provide evidence that CTLA-4 actually served to inhibit the activity of T cells. Since T cells were known to be critical for orchestrating immune attack, Jim and his colleagues hypothesized that perhaps one reason why T cells are not able to attack tumors is because they are being inhibited by CTLA-4. In a landmark Science paper published in 1996, Jim Allison, Max Krummel, and another postdoctoral fellow in the lab Dana Leach, showed that injection of mice with an antibody that blocks CTLA-4 could actually inhibit or eliminate tumor growth in the mice.
ENHANCEMENT OF ANTITUMOR IMMUNITY BY CTLA-4 BLOCKADE
One reason for the poor immunogenicity of many tumors may be that they cannot provide signals for CD28-mediated costimulation necessary to fully activate T cells. It has recently become apparent that CTLA-4, a second counterreceptor for the B7 family of costimu-latory molecules, is a negative regulator of T cell activation. Here, in vivo administration of antibodies to CTLA-4 resulted in the rejection of tumors, including preestablished tumors. Furthermore, this rejection resulted in immunity to a secondary exposure to tumor cells. These results suggest that blockade of the inhibitory effects of CTLA-4 can allow for, and potentiate, effective immune responses against tumor cells.
CHECKPOINT BLOCKADE
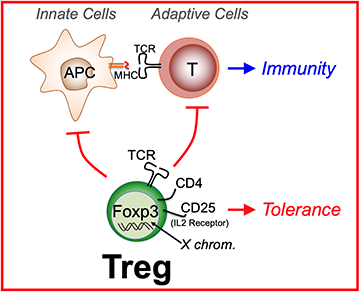
The series of experiments published in the 1996 Science paper represent the birth of a new concept in immunotherapy, the concept of “checkpoint blockade”. The fundamental idea behind checkpoint blockade is that the immune system is normally held in check by inhibitory molecules such as CTLA-4. The inhibitory effects of CTLA-4 are actually very important for the normal function of the immune system, serving as a “checkpoint” that restrains the immune system from inappropriately attacking healthy self tissue. In fact, several groups, including Jim and his colleague Cynthia Chambers, demonstrated the importance of CTLA-4 in restraining the immune system by generating “knockout” mice that completely lack CTLA-4. These knockout animals, which lack CTLA-4 from birth, become very sick at a young age due to hyperactivation of the immune system. However, transient loss of CTLA-4, such as occurs after injection of anti-CTLA-4 antibodies, can lead to a non-fatal and temporary activation of the immune system. The temporary activation of the immune system, though “checkpoint blockade”, provides a window of opportunity during which the immune system is mobilized to attack and eliminate tumors.
THE REST OF THE STORY
Subsequent to his ground-breaking research at UC Berkeley, Jim moved to Memorial Sloan Kettering Cancer Center in New York City to continue his research on CTLA-4 and cancer immunotherapy. He is now at the MD Anderson Cancer Center. Even after publication of the 1996 Science paper, many experts questioned whether anti-CTLA-4 could ever be successfully used in humans. Despite these doubts, and many false starts along the way, the clinical development of anti-CTLA-4 was ultimately taken over by Bristol Myers Squibb, which successfully shepherded anti-CTLA-4 to the clinic under the name Yervoy (Ipilimumab). In 2010, the results of the first phase III clinical trial with Ipilimumab were published in the New England Journal of Medicine. This paper showed that Ipilimumab can significantly prolong the lives of patients with metastatic melanoma that otherwise exhibit a very poor prognosis. Most importantly, perhaps, was the observation that a subset of patients treated with Ipilimumab exhibited long-lasting beneficial effects, in some cases apparently ‘cured’ of their melanoma. Ipilimumab was the first medication to provide durable remissions in a fraction of patients with metastatic melanoma. By no means did everyone benefit from Ipilimumab, but for a field that is hesitant to talk of ‘cures’, these were unexpected and remarkable results. Tumors in patients with metastatic melanoma and many other cancers often acquire resistance to conventional chemotherapy drugs and ultimately re-emerge. In the case of successful immunotherapy, however, it appears that tumors have a much more difficult time acquiring resistance. Another potential advantage of checkpoint therapies is that they may be effective against multiple types of cancer.
It is no exaggeration to claim that the success of Yervoy (Ipilimumab) has now changed the face of cancer therapy. Many drug companies are attempting to develop anti-cancer antibodies with similar modes of action. One particularly promising target for antibodies is a pair of inhibitory molecules, called PD1 and PDL1. Cancer immunotherapy in general has emerged from its exile and is now generating considerable excitement across the pharmaceutical industry.
LESSONS LEARNED
One important lesson to be learned from the story of Ipilimumab is the value of fundamental research. Jim’s original interest in CTLA-4 was driven by his laboratory’s basic curiosity about how T cells are activated and regulated. There was certainly no guarantee at the outset that fundamental research on CTLA-4 would ever lead to a novel therapy for cancer; indeed, it was unlikely that such hope was even at the forefront of the motivation of the researchers that first worked out the role of CTLA-4 in immunity. Instead, these researchers were motivated by a fundamental curiosity about how the immune system works. The winning strategy was to couple curiosity-based research with keeping an eye towards the potential of any findings for the design of new therapies.
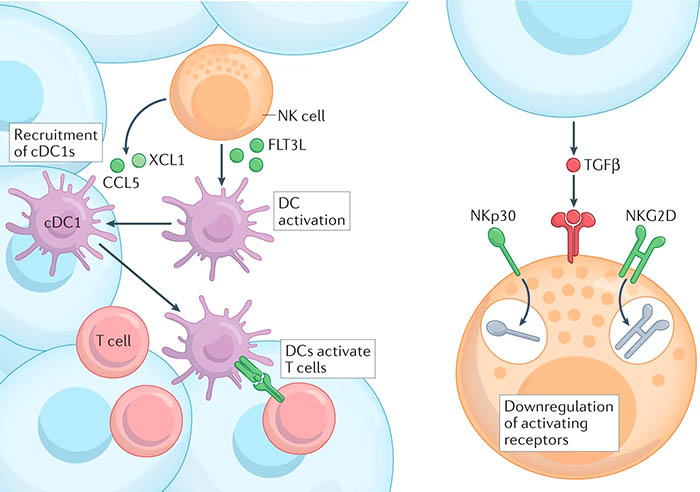
In addition, it is critical to understand that Jim’s work was not performed in isolation. Rather it was based on decades of work, performed in hundreds of laboratories, on the basic architecture and function of T cells and the immune system. Without this fundamental research, Jim’s groundbreaking work would never have been possible. Lastly, given recent and widespread skepticism about the value of mouse models of cancer, it is worth remembering that Jim’s fundamental research, as well as the decades of work leading up to it, was based on and would not have been possible without extensive use of these animal models.
In short, it is impossible to predict which fundamental research will lead to novel therapies and which will not, but what is clear is that fundamental research of all kinds is essential to lay the groundwork for the next breakthrough.
 The Immunotherapeutics and Vaccine Research Initiative is founded on the belief that fundamental research can lead to novel and entirely unexpected approaches to cancer and infectious disease therapies and vaccines. This belief is exemplified by the remarkable story of how research in Molecular and Cell Biology and Public Health
The Immunotherapeutics and Vaccine Research Initiative is founded on the belief that fundamental research can lead to novel and entirely unexpected approaches to cancer and infectious disease therapies and vaccines. This belief is exemplified by the remarkable story of how research in Molecular and Cell Biology and Public Health  CDNs were originally discovered as small molecules produced by bacteria. For many years, CDNs were thought to function solely in bacteria, and their potential value in cancer immunotherapy was not appreciated. This started to change with a 2007
CDNs were originally discovered as small molecules produced by bacteria. For many years, CDNs were thought to function solely in bacteria, and their potential value in cancer immunotherapy was not appreciated. This started to change with a 2007